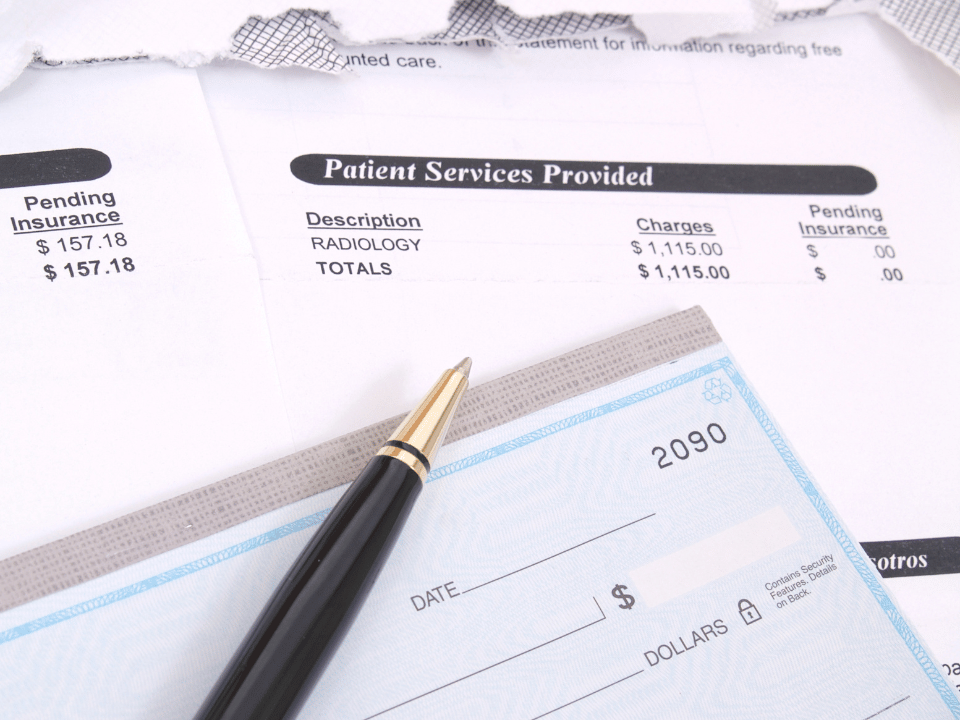
Whether expected or unexpected, medical bills can easily impact financial plans. Medical bills are often confusing, complicated, and often higher than expected.
You may not be aware that medical bills aren’t final and may be disputed. If you think the bill is too high, has erroneous or hidden charges, you can file a dispute with your medical provider. If you want to dispute a medical bill, you’ve come to the right place. Medical billing advocates can work on your behalf to make sense of your medical bills and help negotiate.
What is a Medical Billing Dispute?
Simply put, a medical billing dispute is when a person disagrees with what they are charged for a medical service or procedure. Some of the more common reasons that you may be overcharged or don’t agree with your bill may be due to human error or surprise medical bills. Surprise bills often result from getting emergency treatment or care from someone outside your insurance network. When this happens, the bills are often much higher and unexpected than what you would get charged under normal circumstances.
Since the enactment of the No Surprises Act of 2022 there’s now federal laws that protect people against surprise billing. As a result, there are fewer disputes related to surprise bills. However, whether your medical bill comes as a surprise or not, you have the right to dispute it.
No Surprises Act
The “No Surprises Act” went into effect on January 1, 2022. This act helps to protect patients from surprisingly high medical bills for the services they receive. If you’re insured through your employer, a Marketplace Plan or an individual health plan this law:
– Bans surprise bills for most emergency services, even if you get them out-of-network and without approval beforehand (prior authorization).
– Bans out-of-network cost-sharing (like out-of-network coinsurance or copayments) for most emergency and some non-emergency services. You can’t be charged more than in-network cost-sharing for these services.
– Bans out-of-network charges and balance bills for certain additional services (like anesthesiology or radiology) furnished by out-of-network providers as part of a patient’s visit to an in-network facility.
– Requires that healthcare providers and facilities give you an easy-to-understand notice explaining the applicable billing protections, who to contact if you have concerns that a provider or facility has violated the protections, and that patient consent is required to waive billing protections (i.e., you must receive notice of and consent to being balance billed by an out-of-network provider).
If you’re uninsured or decide to self-pay, this law then requires you to be provided with a “good faith” estimate of how much your care will cost BEFORE you get care.
When patients receive a bill that is significantly different from their estimate, there are specific options they have to help remedy the situation. Of course, navigating these laws can be difficult for many patients, but there is legal recourse to help. However, do not forget that the Emergency Medical Treatment and Active Labor Act (EMTALA) ensures that you are provided with a medical screening examination (MSE) and stabilization if you have an emergency medical condition at Emergency Department’s without consideration of your ability to pay or possible costs.
What to Consider Before Challenging Medical Bills
There are several critical factors that patients should consider before starting down the road of a challenge to their medical bills. Spending some time to understand those considerations before you start the process can lead to better outcomes, and a much smoother overall process.
Know Your Eligibility for Dispute Resolution
If you’re considering using the dispute resolution process set out by the No Surprises Act, there are some qualifying criteria that will allow you to use this process. Those criteria include:
- You didn’t use your insurance to pay for the procedure (You were either uninsured or had insurance, but didn’t use it for the procedure or service).
- Your care occurred on or after January 1, 2022.
- Your provider gave you a good faith estimate
- Your most recent bill is from the last 4 months (120 calendar days).
- The difference between the estimate and final bill from any provider or facility is at least $400.
Understand Your Explanation of Benefits (EOB)
Your explanation of benefits is a letter or statement provided by your insurance company that goes through different factors of your care. This includes what the insurance was charged for the procedure, what the insurance company paid, and what amount you are responsible for paying to the provider or facility.
The explanation of benefits is not a bill. The actual bill will come from the facility or individual provider. It is important to keep your EOBs to ensure that what you’re billed from the provider matches what was paid by the insurance company.
8 Steps on How to Dispute High-Cost Medical Bills
Now that you know that all medical bills are open to dispute let’s look at how to follow through with the process.
1. Gather Information on Your Medical Bills
One of the first reasons that individuals look into challenging a medical bill is because their first reaction to the cost of the bill is that it is outrageous. There are a variety of tools online that allow individuals to get cost comparisons about their medical care. This includes tools from FAIR Health, and the Healthcare Bluebook to give you an estimate of what is typical in your location.
2. Request an Itemized Bill and Review for Errors
You should first get an itemized bill showing a complete list of services and treatments for which you’re getting charged. Once you have the itemized list, you can check for errors such as:
- Duplicate or repeat charges
- Illegal surprise charges
- Billing errors
- Incorrect treatments
- Hidden fees
In addition to being astronomically high, medical bills often need to be clarified and made easier to read. By getting an itemized list, you can double-check that you’re getting charged for the correct treatment(s) or procedure(s).
3. Talk to Your Provider’s Medical Billing Department
Once you understand your medical bill, you know what you’re negotiating. The information allows you to contact your medical provider and ask them for a lower rate or discounted medical bill. While you can ask them for discounts under any circumstances, you’ll have a better chance of getting them if you prove you’re overpaying. Additionally, if you feel there is a mistake in your bill, you can have your provider explain those costs. You can also request a review so they can fix any mistakes.
4. Get in Contact With Your Insurer
If you are still negotiating with your medical provider, your next stop should be your insurance company. In addition to an itemized list of services from your medical provider, you should also receive a list and explanation of benefits from your insurance provider. Upon reviewing your list of benefits, you’ll have a better idea of what your insurance company will and will not pay.
If you don’t think they’re paying for everything they’re supposed to, you can file an appeal with them. You can also file an appeal if they aren’t reimbursing you for out-of-pocket expenses incurred during treatment. Typically, you’ll only have up to 6 months to file an appeal.
5. File an Appeal with Your Insurance Company
You can contact your insurance company if you feel that there is an error in the bill, or if you feel that the provider isn’t following the No Surprises Act. Additionally, Centers for Medicare and Medicaid Services (CMS) has a dedicated hotline that is open seven days a week to field questions and complaints, the No Surprises Help Desk (1-800-985-3059).
6. Push Back Against Coercive Credit Reporting
Depending on who your medical provider is, they may have outsourced your medical bill to a collection agency. When this happens, you must file an appeal with the collection agency and explain the situation to them. Typically, your bill will only get transferred if some amount of time has passed after you were billed and you have not reached out to the provider.
Kindly explain to the collection agency that you’re disputing the bill and see if they will wait to collect it or get the court involved until the dispute gets resolved.
Debt collectors cannot report a medical bill to the credit reporting bureaus without first trying to collect the debt from you. Typically, debt collectors just hope that you’ll pay the bill without question, but you have the right to dispute the information. Furthermore, debt collectors are bound by the Fair Debt Collection Practices Act and you may want to research your applicable rights under the law.
7. Get Help from Your Patient Advocate
In most parts of the country, hospitals and medical facilities have patient advocates available upon request. Patient advocates get employed by the medical facility to act on behalf of the patients they’re treating. They can help you with insurance appeals and information, filing a dispute with the medical provider, and helping as you review your bill and list of benefits.
8. Enlist the Services of a Medical Billing Advocate
While patient advocates are a big help, they are often spread thin throughout the hospital and sometimes need to dedicate more time and energy to your case. When this happens, the best way to dispute a medical bill is with the help of a medical billing advocate. Medical billing advocates are health care advocates with intimate knowledge of the medical billing system and billing codes.
Here are some ways a medical billing advocate can help you dispute a medical bill.
- Spot errors with your medical bill much quicker and easier than you would.
- Negotiate on your behalf with your medical provider to get a discounted bill.
- Negotiate with your insurance company to ensure they’re paying for everything they’re supposed to.
- Help you understand confusing medical bills.
- Help you formulate a plan of attack when you dispute your medical bill.
- Assist you as you set up a repayment plan that fits your budget.
Medical billing advocates also have a better knowledge of medical billing and revenue codes than patient advocates. Our sole job revolves around ensuring a medical bill is discounted and holding your medical provider and insurance companies accountable. While many people turn to medical billing advocates as a last resort, you should contact us immediately if you want to dispute a medical bill because time is of the essence.
